Should you go private?
The 44.5% of Australians who have private health insurance (PHI) for hospital treatment can choose to use that insurance to completely or partially fund their stay in a public or private hospital.
When should a Medicare card holder, eligible for free treatment as a public patient in a public hospital, who also has PHI hospital membership, elect to use it?
Less than 10 % of the time appears to be what is acceptable to the healthcare system.
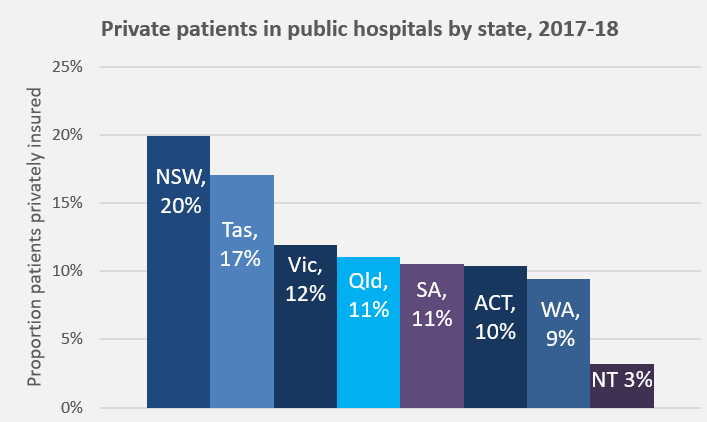
This figure is based on the status quo. In 2006-07, an average of 8.2 % of patients admitted to public hospitals used PHI (essentially rural/remote patients with limited choice and certain specialists who need to work in a public facility). As that figure has increased over time, reaching 13.5 % nationally in 2017-18, it has become a topic of concern, regularly debated and considered unsustainable#.
 Unfortunately, individual patient needs do not really feature in the discussions. Analyses of which type of patients, procedures, and waiting times have contributed to the increase, and reporting of coercive techniques being used on patients to elect PHI, all point back to assumed financial benefit as the driver.
Unfortunately, individual patient needs do not really feature in the discussions. Analyses of which type of patients, procedures, and waiting times have contributed to the increase, and reporting of coercive techniques being used on patients to elect PHI, all point back to assumed financial benefit as the driver.
Public hospitals welcome private patients as they bring funds from an alternate source, and hence save money in their budgets. However, according to a 2018 Report by Martyn Goddard on Tasmanian public hospitals, ‘for each patient admitted as private, the public hospital loses an average of $1,800, compared with treating the same patient publicly‘. He notes that it is a myth that private patients contribute additional funds into public hospitals because the hospital only gets PHI payment for the treatment (that does not cover infrastructure, administration, catering etc. costs) and the Federal Government does not fund these patients with the usual percent of the national efficient price, on the basis that it already pays for Medicare and the private insurance rebate. So the hospital gets only a fraction of the usual activity-based funding**.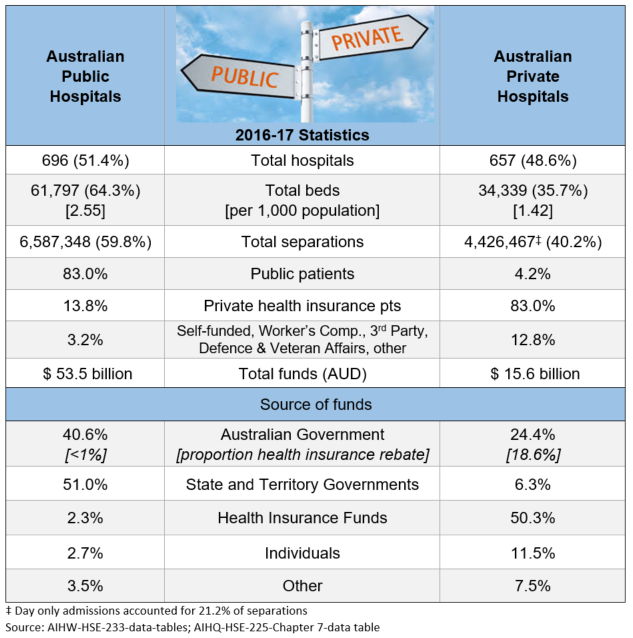
Patients think they are doing the right thing by using their PHI and assisting the public system to free up resources to treat more public patients or conduct research. However, they actually open themselves up to additional costs via excess/co-payments and out-of-pockets from gap specialist charges.
Whatever the altruistic motivations of this cost-shifting to the private sector, it results in upward pressure on insurance premiums. This then sets off a sequence of events to rival ‘Mouse Trap’, except everyone seems to get caught with the cheese at the end. When PHI premiums go up, people drop their private health insurance. These people then rely on the public health system and the health insurance rebate age penalty actively works against them opting back into private insurance at a later date.
The more privately insured people who use their cover in public hospitals, then the less beds are available for public patients and waiting times go up in the public hospital system producing a political issue for both State and Federal Governments. Some public patients are shunted to private facilities (this already happens at a pretty constant rate of 4% of separations per annum).
In reality, these are no true private hospitals, rather a symbiotic relationship exists between public and private across the Australian healthcare system. The table shows that PHI accounted for 50.3 % of private hospital funding in 2016-17. A further 30 % coming from Federal and State Governments, including Medicare payments for medical services and the private health insurance rebate.
