Primary care organisations in Australia
The development of primary care organisations since the 1980s is based on evidence that a well-developed primary care model improves health outcomes and cost-effectiveness in the whole healthcare system. A key being their increasing use to implement public health care reforms including shifting services away from hospital settings and into the community.
Primary healthcare in Australia is provided mainly by independent general practitioners (GP) on a fee-for-service basis, predominantly funded by the Australian Government through Medicare. Over 80% of GP services are bulk-billed, with the doctor accepting a Government reimbursed schedule fee as full payment. There is no system of patient registration with a GP or practice, and patients may consult any GP.
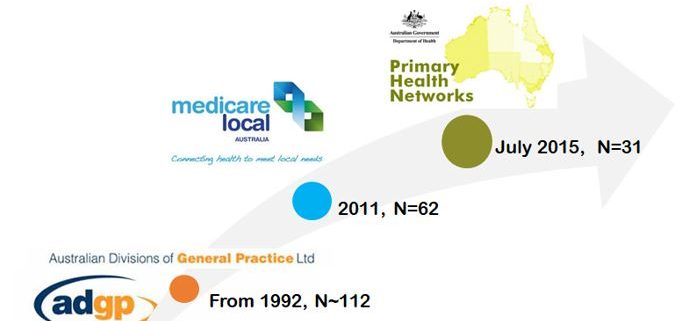
The first major structural reform in Australian primary care was the establishment of Divisions of General Practice from 1992. At their zenith, there were 119 nationally with 94% of GPs as members. Additional reforms included a practice incentive programme to improve quality and accountability of GP services such as paying for immunisations and prescribing reviews; a rural incentives programme that includes paying GPs to relocate to and stay in rural and remote communities and outer urban areas; and amendments to the fee schedule that encourage participation in care planning and case conferencing and more multidisciplinary care.
In 2008, the then Labor government established the National Health and Hospital Reform Commission (NHHRC) to conduct a comprehensive review of Australia’s health system. The final report gave rise to the Council of Australian Governments’ (COAG) National Health Reform Agreement (2011). The Commonwealth Government agreed to fund a new primary healthcare structure to improve coordination and integration of primary health care in local communities, address service gaps, and make it easier for patients to navigate their local health care system.
The establishment of 61 Medicare Locals across Australian regions aimed to strengthen the primary care system (and thereby relieve pressure on hospitals and other acute providers). Medicare Locals were non-profit companies selected after a competitive application process and funded largely by the Commonwealth with $1.8 billion for the period 2011–12 to 2015–16.
Many GPs saw the new structures as a threat to their primacy in their local primary care market and an unnecessary additional layer of bureaucracy. This negative view was reinforced by the Australian Medical Association, that lobbied the Coalition Opposition on the basis of the perceived threat to the GP small businesses.
Not surprisingly, soon after coming into office, the new Minister for Health, Peter Dutton, announced a review of Medicare Locals. Conducted by Professor John Horvath, assisted by two consulting firms, the review informed the 2014-15 Budget announcement that all Medicare Locals would cease operation on 30 June 2015 and a new network of Primary Health Networks (PHNs) would be established.
Despite the significant costs associated with winding up the relatively recently established Medicare Locals, and a poorly managed public tender process, on 1 July 2015, 31 PHNs, funded by approximately $900 million, replaced the Medicare Locals.
PHNs are independent organisations funded by the Australian Government. They work collaboratively with local hospital networks (LHNs), and their boundaries closely align. Each PHN is overseen by a board. The board is advised by a GP-led clinical council and a community advisory committee.
The new PHNs are responsible for populations and geographic areas that are much larger than those of the Medicare Locals. While Medicare Locals had an average population of 355,000; PHNs service an average population of 738,000.
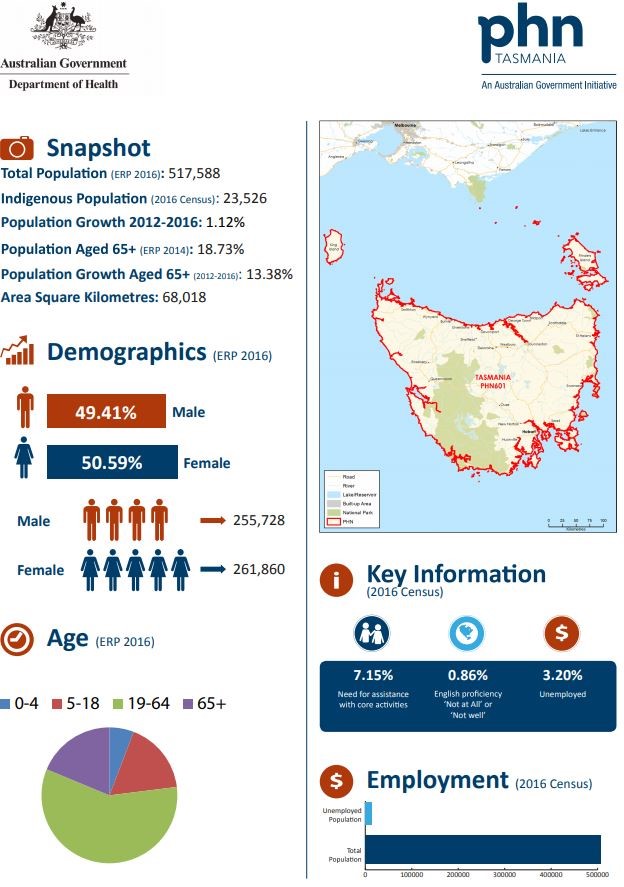
An example snapshot of Tasmanian PHN is provided. Refer to the PHN website for further information and links to individual PHNs.